The widely held belief that depression is due to low levels of serotonin in the brain – and that effective treatments raise these levels – is a myth, argues a leading psychiatrist in The BMJ this week.
David Healy, Professor of Psychiatry at the Hergest psychiatric unit in North Wales, points to a misconception that lowered serotonin levels in depression are an established fact, which he describes as “the marketing of a myth.”
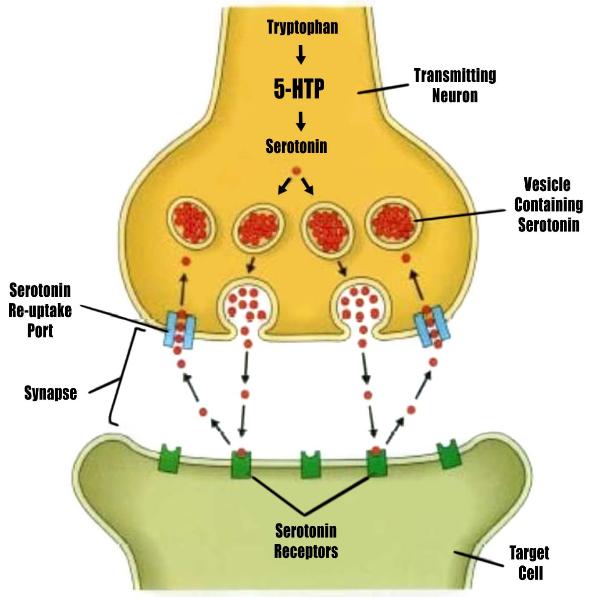
The serotonin reuptake inhibiting (SSRI) group of drugs came on stream in the late 1980s, nearly two decades after first being mooted, writes Healy. The delay centred on finding an indication.
After concerns emerged about tranquilliser dependence in the early 1980s, drug companies marketed SSRIs for depression, “even though they were weaker than older tricyclic antidepressants, and sold the idea that depression was the deeper illness behind the superficial manifestations of anxiety,” he explains. The approach was an astonishing success, “central to which was the notion that SSRIs restored serotonin levels to normal, a notion that later transmuted into the idea that they remedied a chemical imbalance.”
In the 1990s, no one knew if SSRIs raised or lowered serotonin levels, he writes; they still don’t know. There was no evidence that treatment corrected anything, he argues.