Videos :
Anecdotals (5:22 – 18:30)
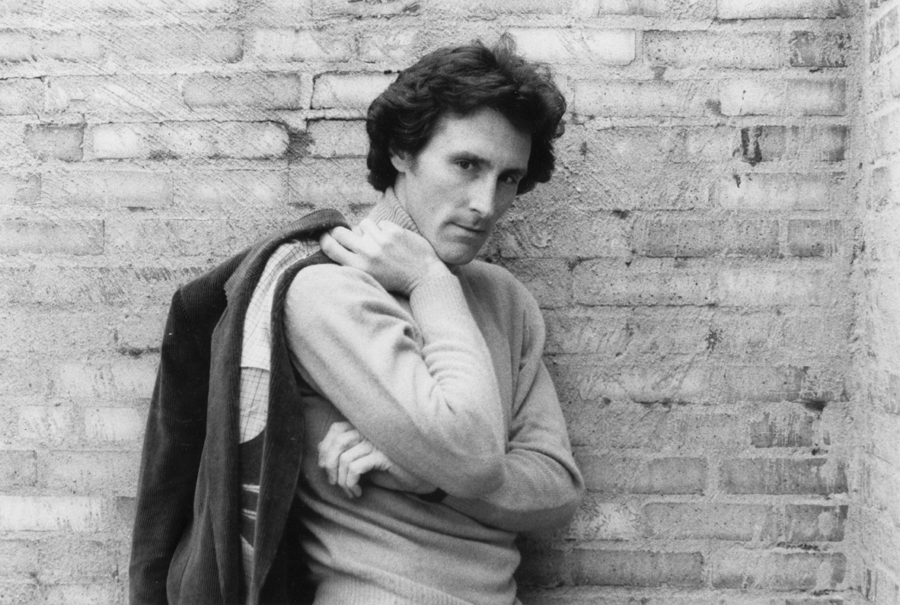
Getting Healthy With Gary Null: Actor Fred Fischer (6:31)
Olive leaves contain natural treatment for endometriosis, study reveals
Baylor College of Medicine, December 15, 2022
Olive leaves may hold the key to treating women with endometriosis. The debilitating condition affects up to 15 percent of women of reproductive age in the United States alone and millions worldwide. Endometriosis is a disease which sees women develop tissue resembling endometrium (the lining of the uterus) outside the uterus. It causes chronic inflammatory that can lead to the formation of scar tissue within the pelvis and other areas. Due to estrogen’s close link to the condition, current targets have so far aimed to systematically remove estrogen and use anti-inflammatory drugs. The issue is that these drugs aren’t very effective and may even result in adverse side-effects. Han and his team have now set out to find more effective options. Previously, Han has shown that estrogen receptor-beta (ER-beta), which is one of two receptors that mediate estrogen’s effects on cells alongside estrogen receptor-alpha (ER-alpha), contributes significantly to the condition’s progression. Han and his team have worked with cell cultures in their lab and extensively browsed a library of natural products, looking for compounds that could act as non-hormonal treatment options for the condition. They found that oleuropein, a naturally-occurring compound found in olive leaves, can selectively inhibit ER-beta activity, but not ER-alpha activity. Further, oleuropein was able to suppress the growth of endometriosis lesions in mice without inducing harm.“In addition, oleuropein treatment was neither toxic to the liver nor did it affect the ability of female mice to have offspring,” Han says. “In mice with endometriosis, oleuropein improved the pregnancy rate. Oleuropein is less expensive than hormonal therapy, and our current findings suggest that it is safer than current treatments.”
(NEXT)
More exercise linked to less-severe COVID-19 outcomes
Kaiser Permanente, December 15, 2022
Kaiser Permanente members who were more physically active prior to being diagnosed with COVID-19 had a lower risk of severe outcomes, according to research published in the American Journal of Preventive Medicine. The study of nearly 200,000 adults showed an association between physical activity and improved COVID-19 outcomes across major demographic groups regardless of whether patients had chronic medical conditions. Black, Hispanic, and Asian patients had a greater risk of adverse outcomes compared with white patients, in line with prior research. However, within each racial and ethnic group, more exercise was still associated with less severe COVID-19 outcomes. “The main message is that every little bit of physical activity counts,” said the study’s lead author, Deborah Rohm Young, Ph.D., the director of the Division of Behavioral Research for the Kaiser Permanente Southern California Department of Research & Evaluation. “The more exercise the better, no matter a person’s race, ethnicity, age, sex, or chronic conditions.” In this study, Young and her colleagues analyzed the electronic health records of 194,191 adult patients at Kaiser Permanente in Southern California who were diagnosed with COVID-19 between January 2020 and May 2021, prior to widespread COVID-19 vaccination. All patients had reported their physical activity levels prior to infection in a routine measure known as the Exercise Vital Sign. Each patient fell into 1 of 5 categories ranging from always inactive—10 minutes of exercise or less per week, to always active—150 minutes of exercise per week. Statistical analysis showed that the more physical activity a patient reported, the lower the risk of hospitalization or death within 90 days of COVID-19 diagnosis. This trend was consistent across all activity levels, with always-active patients facing the lowest risk. More exercise was also linked to lower rates of hospitalization or death for patients with certain underlying chronic conditions—such as hypertension, cardiovascular disease, or obesity—that are typically associated with an increased risk of poor COVID-19 outcomes.
(NEXT)
Could glucosamine and chondroitin support a healthy colon?
Memorial Sloan Kettering Cancer Center, December 7, 2022
Supplements of glucosamine and chondroitin may support colon health via an anti-inflammatory mechanism, according to data from two big US cohorts. Use of the supplements, which are used for joint health support, was associated with a 23% reduction in the risk of colorectal cancer, according to data from the Nurses’ Health Study and Health Professionals Follow-up Study published in the International Journal of Cancer .“Results of this study suggest a potential beneficial effect of glucosamine and chondroitin supplementation on risk of colorectal cancer, and further support the previously observed association between use of these supplements and risk of colorectal cancer in the VITAL study,” wrote the researchers. The new study, led by Dr Elizabeth Kantor from the Memorial Sloan Kettering Cancer Center in New York, analyzed data from 68,466 women and 27,934 men participating in the Nurses’ Health Study and Health Professionals Follow-up Study, respectively. This yielded 672 cases of colorectal cancer. After crunching the numbers, the researchers found that any use of glucosamine was associated with a 21% reduction in risk, while any use of chondroitin was associated with a 23% reduction in risk. While glucosamine in the absence of chondroitin did not show an effect, use of glucosamine + chondroitin was significantly associated with a 23% reduction in risk, wrote Dr Kantor and her co-workers. The results did not change significantly when the researchers factored in sex, BMI, or physical activity, and the association was comparable when the researchers split the cancers according to colon and rectum.
(NEXT)
Poor gut health may drive multiple sclerosis—better diet may ease it
Rutgers University, December 15, 2022
Researchers from Rutgers Robert Wood Johnson Medical School’s Department of Neurology have traced a previously observed link between microscopic organisms in the digestive tract—collectively known as the gut microbiome—and multiple sclerosis (MS). Their study in genetically altered mice and people supports the belief that dietary adjustments such as increased fiber may slow MS progression, and they are already working to test the effect of dietary interventions in MS patients. The Rutgers study, which was led by research associate Sudhir Kumar Yadav, used mice engineered with MS-associated genes to trace the link between alterations in the gut bacteria and an MS-like condition called experimental autoimmune encephalomyelitis (EAE). As these mice matured—and simultaneously developed EAE and a gut inflammatory condition called colitis—the researchers observed increased recruitment of inflammatory cells (neutrophils) to the colon and production of an anti-microbial protein called lipocalin 2 (Lcn-2).
The study team then looked for evidence that the same process occurred in people with MS and found significantly elevated Lcn-2 levels in patient stool. This marker correlated with reduced bacterial diversity and increased levels of other markers of intestinal inflammation. Additionally, bacteria that seem to ease inflammatory bowel disease were reduced in MS patients with higher levels of fecal Lcn-2. The study suggests that fecal Lcn-2 levels may be a sensitive marker for detecting unhealthy changes in the gut microbiome of MS patients. It also provides further evidence that high-fiber diets, which reduce gut inflammation, may help fight MS.
(NEXT)
Stressed about college finals? Eat a handful of walnuts
University of South Australia, December 14, 2022
Being a university student can sometimes feel like your stress level will never go down and the workload will never end. However, new research finds that eating just two ounces of walnuts per day may be able to help counteract the harmful effects of academic stress. To explore the potential effects of dietary interventions, Larisa Bobrovskaya, PhD, Associate Professor of Clinical and Health Sciences at the University of South Australia conducted a randomized controlled trial with 60 university students between 18 and 35 years-old, randomly selected to be in either a treatment group or control group for 16 weeks. The treatment group had to consume 56 grams of walnuts daily while the control group did not consume any nuts or fatty fish. The students provided blood and saliva samples and completed questionnaires to give the team insight on their mental health, mood, overall well-being, and sleep habits at three different times throughout the study. Some participants also provided fecal samples during each visit. From their experiments, the researchers found that eating walnuts daily prevented worrisome shifts in mental health-related scores for stress and depression. It also appeared to improve metabolism by increasing total protein and albumin levels, which can also be protective against the harms of academic stress. Walnut consumption even helped to improve sleep, according to the students’ self-reports. These findings are consistent with other clinical and observational studies that link walnuts with lowering the frequency of depressive symptoms, improving mood, and reaching better overall health at an older age. In light of this, the study authors are even more proud of what their work has contributed to the body of evidence.
(NEXT)
Exercise is medicine for cancer and every dose counts, even in late stages of the disease: Study
Edith Cowan University (Australia), December 14, 2022
It is well-known that exercise has many benefits, but new Edith Cowan University (ECU) research has revealed just how critically important it can be—even for people with advanced cancer. Previous work from ECU’s Exercise Medicine Research Institute has shown men with advanced prostate cancer can change the chemical environment of their body over six months of exercise training to suppress the growth of cancer cells. The team observed increased levels of proteins called “myokines” which are produced by skeletal muscles and can suppress tumor growth and even help actively fight cancerous cells by stimulating a range of anti-cancer processes in the body. But a new EMRI study has shown a single bout of exercise can elevate myokines even further and induce additional cancer suppression. Importantly, this exercise-induced effect occurs in patients with incurable, advanced cancer where the disease has well and truly taken hold and patients have already received extensive treatment over many years. Nine patients with late-stage prostate cancer performed 34 minutes of high intensity exercise on a stationary cycle, with blood serum collected immediately before and after, and then again 30 minutes post-workout. The team found the serum obtained immediately after this session of exercise contained elevated levels of anti-cancer myokines resulting in suppressed growth of prostate cancer cells in vitro by about 17%. Serum myokine levels and cancer suppression returned to baseline after 30 minutes.